Angiotensin Converting Enzyme Lab Test
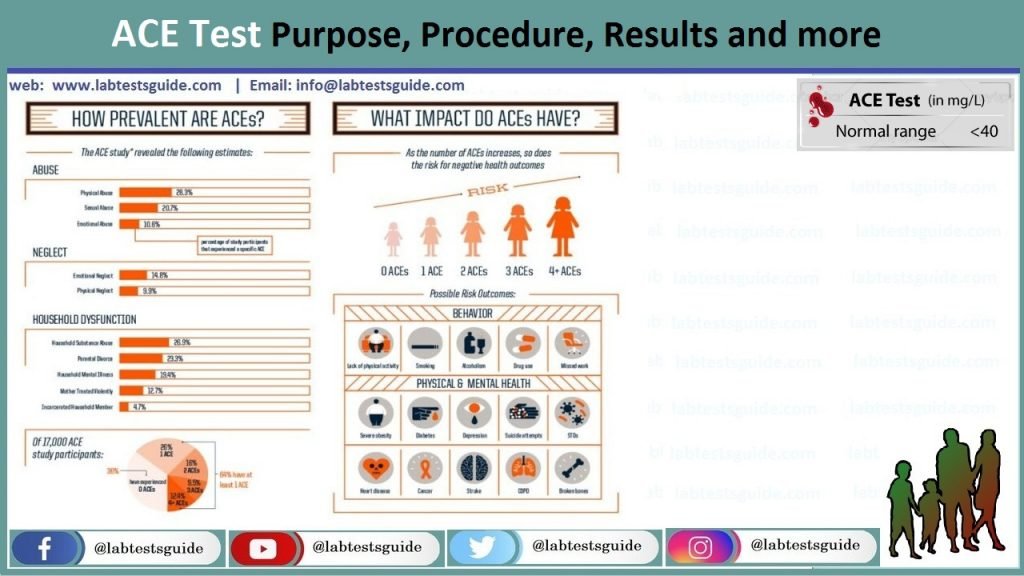
In the realm of cardiovascular diagnostics, the angiotensin-converting enzyme (ACE) lab test stands as a crucial tool for clinicians. This assay quantifies the serum concentration of ACE, a carboxypeptidase that plays a pivotal role in the renin-angiotensin-aldosterone system (RAAS). By catalyzing the conversion of angiotensin I to angiotensin II, ACE contributes to vasoconstriction, blood pressure regulation, and fluid balance. However, elevated or depressed ACE levels can signify underlying pathologies, making this test indispensable in differential diagnosis.
The Biochemical Underpinnings of ACE

The RAAS is a complex hormonal cascade initiated by renin release from the kidneys. Renin cleaves angiotensinogen into angiotensin I, which is then converted to angiotensin II by ACE. Angiotensin II binds to AT1 receptors, triggering aldosterone secretion from the adrenal cortex, which in turn promotes sodium and water retention in the kidneys. This intricate system is essential for maintaining blood pressure homeostasis, but dysregulation can lead to hypertension, heart failure, and other cardiovascular disorders.
Clinical Indications for ACE Testing

Physicians order the ACE test in various clinical scenarios, primarily to investigate sarcoidosis, a granulomatous disease of unknown etiology. Elevated ACE levels are observed in 50-70% of sarcoidosis patients, particularly those with pulmonary or ocular involvement. However, ACE is not specific to sarcoidosis and may be elevated in other conditions, including:
- Gaucher disease (a lysosomal storage disorder)
- Lymphoma
- Tuberculosis
- Hyperthyroidism
Conversely, decreased ACE levels are associated with:
- Cushing's syndrome (due to glucocorticoid-induced suppression)
- Hypothyroidism
- Acute liver disease
- Use of ACE inhibitors (e.g., lisinopril, enalapril)
Methodology and Reference Ranges
The ACE assay is typically performed using spectrophotometric or fluorometric methods. The most common technique involves measuring the enzyme’s activity by monitoring the hydrolysis of a synthetic substrate, such as hippuryl-histine-leucine. The reaction rate is proportional to ACE concentration.
| Population | Reference Range (U/L) |
|---|---|
| Adults | 8-53 |
| Children | 15-80 |

Limitations and Confounding Factors
Several factors can influence ACE levels, potentially leading to false positives or negatives:
- Pregnancy (especially third trimester)
- Chronic obstructive pulmonary disease (COPD)
- Alcohol consumption
- Use of oral contraceptives
- Aspirin therapy
- Acute phase of infections
Case Study: ACE Testing in Sarcoidosis

A 42-year-old female presents with chronic cough, fatigue, and bilateral hilar lymphadenopathy on chest X-ray. Her ACE level is 85 U/L (reference range: 8-53 U/L). While the elevated ACE supports a diagnosis of sarcoidosis, the clinician orders additional tests, including a gallium scan and bronchoscopy with biopsy, to confirm the diagnosis. This case illustrates the importance of using ACE as a complementary tool rather than a standalone diagnostic test.
Future Directions: ACE and Personalized Medicine
Emerging research suggests that ACE polymorphisms, particularly the insertion/deletion (I/D) variant, may influence individual susceptibility to cardiovascular diseases and response to ACE inhibitor therapy. The D allele is associated with higher ACE levels and increased risk of hypertension, whereas the I allele may confer protection. As our understanding of genetic determinants deepens, ACE testing could evolve into a component of personalized medicine, guiding tailored therapeutic interventions.
What is the normal range for ACE levels in adults?
+The normal range for ACE levels in adults is typically 8-53 U/L, although this may vary slightly between laboratories.
Can medications affect ACE test results?
+Yes, medications such as ACE inhibitors, oral contraceptives, aspirin, and glucocorticoids can significantly alter ACE levels, potentially leading to false results.
Is the ACE test specific for sarcoidosis?
+No, while elevated ACE levels are common in sarcoidosis, they are not specific and can be observed in other conditions, necessitating additional diagnostic tests for confirmation.
How is the ACE test performed?
+The ACE test is typically performed using spectrophotometric or fluorometric methods, measuring the enzyme's activity by monitoring the hydrolysis of a synthetic substrate.
What are the limitations of ACE testing?
+ACE testing has limitations, including lack of specificity, influence of medications and medical conditions, and variability in reference ranges between laboratories.
In conclusion, the angiotensin-converting enzyme lab test is a valuable diagnostic tool with broad applications in cardiovascular and pulmonary medicine. While its utility is most pronounced in sarcoidosis, clinicians must remain cognizant of its limitations and interpret results within the broader clinical context. As our understanding of ACE biology expands, this assay may play an increasingly pivotal role in personalized medicine, informing targeted therapeutic strategies and improving patient outcomes.