What Are Gram Positive Cocci? Identification Tips
Gram-positive cocci are a type of bacteria that are characterized by their spherical or oval shape and their ability to retain the crystal violet stain used in the Gram staining procedure, resulting in a purple color under a microscope. This group of bacteria includes several species that are commonly found in the environment and on the human body, some of which can cause disease.
One of the key identification tips for gram-positive cocci is their morphology, which can be observed under a microscope. These bacteria typically appear as single cells, in pairs (diplococci), or in clusters, and their cell walls are composed of a thick layer of peptidoglycan. The most common types of gram-positive cocci include Staphylococcus and Streptococcus, each with its own distinct characteristics and clinical significance.
Staphylococcus species, such as Staphylococcus aureus, are often found in clusters and can produce a variety of pigments, including golden-yellow carotenoid pigments. These bacteria are commonly associated with skin and soft tissue infections, as well as more severe conditions like bacteremia and endocarditis. In contrast, Streptococcus species, such as Streptococcus pneumoniae, typically appear in pairs or chains and are often associated with respiratory tract infections, including pneumonia and sinusitis.
Another important characteristic of gram-positive cocci is their ability to grow on various types of media, including blood agar and chocolate agar. The pattern of growth, including the size and shape of colonies, as well as the presence of hemolysis (breakdown of red blood cells), can provide valuable clues for identification. For example, Staphylococcus aureus colonies are typically large and golden-yellow, while Streptococcus pneumoniae colonies are smaller and may exhibit a draughtsman or carrom coin appearance.
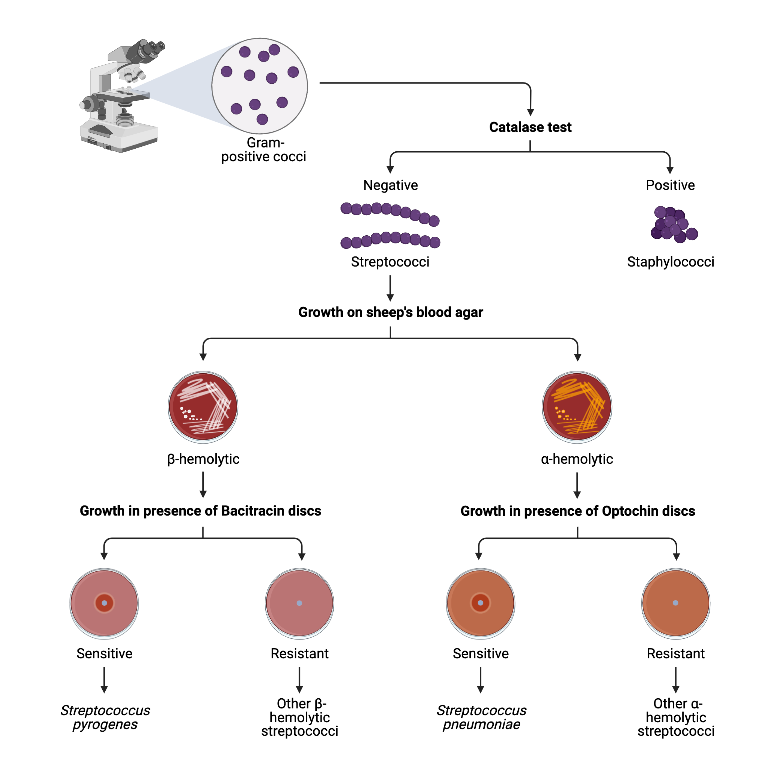
In addition to morphological and cultural characteristics, gram-positive cocci can also be identified using biochemical tests, such as the catalase test and the coagulase test. The catalase test, which detects the presence of the enzyme catalase, can help distinguish between Staphylococcus and Streptococcus species, as Staphylococcus species are typically catalase-positive. The coagulase test, which detects the ability of an organism to coagulate rabbit plasma, is commonly used to identify Staphylococcus aureus, which is coagulase-positive.
Molecular techniques, such as PCR (polymerase chain reaction) and DNA sequencing, can also be used to identify gram-positive cocci. These methods can provide rapid and accurate identification, which is particularly important in clinical settings where timely diagnosis and treatment are critical.
When working with gram-positive cocci, it is essential to follow proper laboratory safety protocols to avoid contamination and ensure accurate results. This includes using sterile equipment and supplies, handling cultures and specimens carefully, and following established procedures for staining, culturing, and biochemical testing.
In conclusion, gram-positive cocci are an important group of bacteria that can be identified using a combination of morphological, cultural, biochemical, and molecular techniques. By understanding the characteristics of these organisms, including their morphology, growth patterns, and biochemical properties, laboratories can provide accurate diagnoses and guide treatment decisions.
What is the difference between Staphylococcus and Streptococcus species?
+Staphylococcus and Streptococcus species are both gram-positive cocci, but they have distinct characteristics. Staphylococcus species, such as Staphylococcus aureus, are often found in clusters and can produce pigments, while Streptococcus species, such as Streptococcus pneumoniae, typically appear in pairs or chains.
How are gram-positive cocci typically identified in the laboratory?
+Gram-positive cocci can be identified using a combination of morphological, cultural, biochemical, and molecular techniques. This may include Gram staining, growth on various types of media, biochemical tests such as the catalase and coagulase tests, and molecular techniques like PCR and DNA sequencing.
What are some common clinical conditions associated with gram-positive cocci?
+Gram-positive cocci, including Staphylococcus and Streptococcus species, can cause a range of clinical conditions. Staphylococcus aureus is commonly associated with skin and soft tissue infections, as well as more severe conditions like bacteremia and endocarditis. Streptococcus pneumoniae is often associated with respiratory tract infections, including pneumonia and sinusitis.
To further illustrate the characteristics of gram-positive cocci, let’s consider a few examples. Staphylococcus epidermidis, a common skin commensal, is often found in clusters and can produce a biofilm that protects it from antimicrobial agents. In contrast, Streptococcus pyogenes, the cause of strep throat, typically appears in chains and can produce a variety of virulence factors, including hemolysins and cytokines.
In terms of prevention and treatment, it is essential to practice good hygiene, including frequent handwashing and proper wound care, to reduce the risk of infection with gram-positive cocci. When infections do occur, antimicrobial therapy may be necessary, and the choice of agent will depend on the specific organism and its susceptibility pattern.
Overall, gram-positive cocci are an important group of bacteria that can cause a range of clinical conditions. By understanding their characteristics, including their morphology, growth patterns, and biochemical properties, laboratories can provide accurate diagnoses and guide treatment decisions.
Gram-positive cocci are a diverse group of bacteria that can be identified using a combination of morphological, cultural, biochemical, and molecular techniques. By understanding the characteristics of these organisms, including their morphology, growth patterns, and biochemical properties, laboratories can provide accurate diagnoses and guide treatment decisions.
As researchers and clinicians continue to study gram-positive cocci, new insights into their biology and clinical significance are likely to emerge. For example, recent studies have highlighted the importance of the microbiome in shaping the behavior of gram-positive cocci, and have identified new targets for antimicrobial therapy.
Looking to the future, it is clear that gram-positive cocci will remain an important area of research and clinical focus. By continuing to advance our understanding of these organisms, we can develop new strategies for prevention, diagnosis, and treatment, and ultimately improve patient outcomes.
To identify gram-positive cocci, follow these steps:
- Obtain a specimen from the patient, such as a blood or tissue sample.
- Perform a Gram stain to determine the morphology and Gram reaction of the organism.
- Grow the organism on various types of media, including blood agar and chocolate agar, to observe its growth patterns and colonial morphology.
- Perform biochemical tests, such as the catalase and coagulase tests, to help identify the organism.
- Use molecular techniques, such as PCR and DNA sequencing, to confirm the identification and determine the organism's susceptibility pattern.
In conclusion, gram-positive cocci are a complex and fascinating group of bacteria that continue to be an important area of research and clinical focus. By advancing our understanding of these organisms, we can develop new strategies for prevention, diagnosis, and treatment, and ultimately improve patient outcomes.
The use of molecular techniques, such as PCR and DNA sequencing, has several advantages, including:
- Rapid and accurate identification of the organism
- Determination of the organism’s susceptibility pattern
- Ability to detect virulence factors and other genetic elements
However, there are also some potential drawbacks, including:
- High cost and complexity of the equipment and reagents
- Need for specialized training and expertise
- Potential for contamination or false positives
