What Does Soap Stand For In Soap Notes
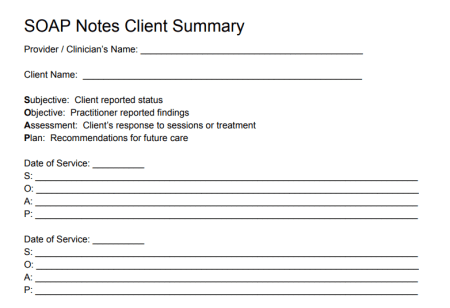
In the context of medical documentation, SOAP notes are a widely used method for recording patient information in a structured and organized manner. SOAP is an acronym that stands for:
- S: Subjective
- O: Objective
- A: Assessment
- P: Plan
This framework allows healthcare professionals to document patient interactions in a clear and concise way, ensuring that all relevant information is captured and communicated effectively among the healthcare team.
Subjective (S)
The subjective section includes the patient’s reported symptoms, feelings, and experiences. This is essentially what the patient tells the healthcare provider about their condition, including their medical history, chief complaint, and any other relevant information they share. It’s the patient’s subjective experience of their illness or condition.
Objective (O)
The objective section contains factual, measurable data that the healthcare provider observes or obtains through diagnostic tests and examinations. This includes vital signs (like temperature, blood pressure, and pulse), laboratory results, physical examination findings, and any other objective data that can be verified.
Assessment (A)
The assessment section is where the healthcare provider interprets the information gathered from the subjective and objective sections to formulate a diagnosis or list of potential diagnoses. This part of the SOAP note requires the healthcare provider to analyze the patient’s symptoms and test results, consider differential diagnoses, and potentially identify the underlying cause of the patient’s condition.
Plan (P)
The plan section outlines the steps to be taken to address the patient’s condition, based on the assessment. This can include treatments, therapies, lifestyle changes, further diagnostic testing, referrals to specialists, patient education, and follow-up appointments. The plan should be specific, achievable, and aligned with the patient’s needs and preferences.
SOAP notes are crucial for maintaining accurate, thorough, and legally sound medical records. They help ensure continuity of care, facilitate communication among healthcare providers, and support high-quality patient care. By following the SOAP structure, healthcare professionals can ensure that their documentation is comprehensive, yet easy to review and understand, making it an indispensable tool in clinical practice.
